This factsheet is for people who have a thoracic aortic aneurysm, or who would like information about it.
A thoracic aortic aneurysm is a widening or bulging of the aorta (the largest blood vessel) in the chest (thorax). It usually occurs at a weak spot in the aortic wall. It may not cause any symptoms, but if the aneurysm widens rapidly it may cause chest pain which can be severe. If it bursts (ruptures) this can be fatal.
About thoracic aortic aneurysms
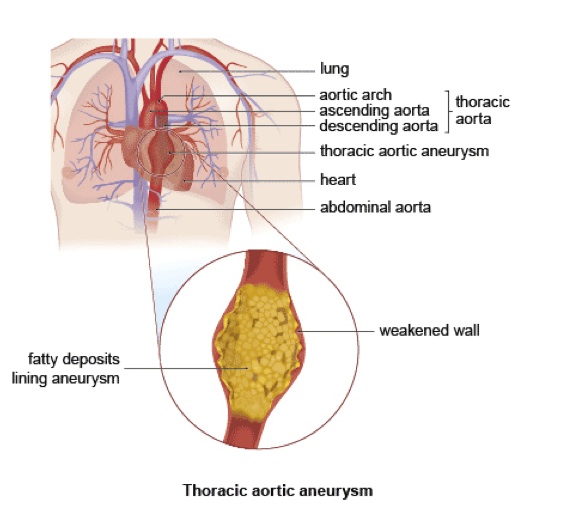
The aorta is the largest artery in your body. It carries all the blood that is pumped out of your heart and distributes it, via its many branches, to all the organs of your body. The aorta passes upwards from your heart before curving backwards and downwards and travelling through your chest (the thoracic aorta) and into your abdomen (the abdominal aorta).
The aorta is usually 2 to 3cm (about one inch) in diameter. A weak spot in the aorta can cause it to bulge outwards (called an aneurysm). If the bulge occurs in the aorta as it goes through your chest, it’s called a thoracic aortic aneurysm. If it occurs in the aorta as it goes through your abdomen, it’s called an abdominal aortic aneurysm (AAA). AAAs are more common than thoracic aneurysms. For more information, see abdominal aortic aneurysm.
The chance of an aneurysm rupturing depends on its size. If your aneurysm is greater than 5.5cm wide the chances of rupture are high – and the risk increases with increasing size.
Symptoms of thoracic aortic aneurysm
A thoracic aortic aneurysm often causes no symptoms. However, if it starts to expand and push on surrounding tissue or nerves in your chest, it can cause:
chest pain (as the aneurysm widens the pain will spread into your upper back) back pain difficulty breathing coughing
wheezing hoarseness difficulty swallowing
These symptoms aren’t always caused by thoracic aortic aneurysms but if you have them, you should see your doctor.
Complications of thoracic aortic aneurysm
Complications of thoracic aortic aneurysm can include the following.
Heart failure – if the aneurysm occurs near your heart it may cause the aortic valve to leak. This can cause blood to flow back into your heart (called aortic regurgitation) and stop your heart pumping effectively and cause heart failure.
Aortic dissection – very rarely, the inner lining of the aorta tears and blood enters the wall of the aorta separating the layers that make up the aortic wall. If this happens, you may feel sudden and excruciating chest and back pain.
Rupture – if the aneurysm ruptures it causes severe internal bleeding and can be fatal without emergency surgery to repair it. The risk of an aneurysm rupturing increases as it gets wider.
Causes of thoracic aortic aneurysm
The main cause of thoracic aortic aneurysm is atherosclerosis. This is a process in which fatty deposits build up on the inside of your arteries and weaken the artery walls.
You are more likely to develop atherosclerosis, and therefore an aneurysm, if you:
smoke are over 50 have a family history of aneurysms have high blood pressure do little physical activity have high cholesterol are overweight
Your risk of having an aneurysm increases if you have:
Marfan’s syndrome
syphilis – this can lead to aortic regurgitation and aortic aneurysm in its late stages if it isn’t treated (this may happen 10 to 20 years after the initial infection)
Diagnosis of thoracic aortic aneurysm
Aortic aneurysms often don’t have any symptoms, unless they are large or are expanding quickly. Your GP may only suspect you have an aneurysm following a routine examination. If your doctor suspects an aortic aneurysm, you may have other tests in hospital, including the following.
Chest X-ray – this may show a widening of your aorta.
Transthoracic echocardiography – an ultrasound sensor is placed over your chest so that your heart and thoracic aorta can be seen working.
Transoesophageal echocardiography – a small ultrasound sensor is passed into your oesophagus or gullet (the food pipe that goes from your mouth to your stomach).
CT or MRI scan – these provide a detailed three-dimensional image of the thoracic aorta and are very useful for determining the exact position of the aneurysm.
Contrast aortography – a special dye is injected into your blood stream. The dye shows up the aorta and any aneurysms on an X-ray image.
Screening
At present there is no national screening programme to detect thoracic aortic aneurysms, only abdominal aortic aneurysms. However, ultrasound scans to screen for the condition are available from private clinics and hospitals.
Treatment of thoracic aortic aneurysm
Your treatment for thoracic aortic aneurysm will depend on your symptoms and the size of your aneurysm.
Watchful waiting
If you have a small aneurysm, surgery isn’t usually advised but you will need regular ultrasound checks to see if your aneurysm is expanding. It’s also important to manage your condition by changing your lifestyle and treat any condition that may be causing the aneurysm (such as high blood pressure).
Surgery
Elective or planned surgery is often advised if your aneurysm is:
larger than 5.5cm expanding by more than 1cm per year causing any symptoms
There are two main surgical options for thoracic aortic aneurysm. Both are usually performed under general anaesthesia. This means you will be asleep during the operation.
Open surgery
This is the traditional method of treating aneurysms. It’s a major operation in which your surgeon opens your chest to access the aorta and inserts a graft into the weak area of the aorta. The graft can be either a piece of blood vessel taken from another place in your body or it can be synthetic. A synthetic graft is made out of an elastic material and is similar to your normal healthy aorta. The blood flows through the graft inside the aorta instead of going through the aneurysm and prevents the aneurysm from getting bigger. For more information, see open surgery for aortic aneurysm.
The operation can be done using keyhole surgery. Keyhole surgery is less invasive and involves making two or three small cuts on your chest. Your surgeon will insert a tube-like telescopic camera, which will send pictures to a monitor so he or she can see the aneurysm. Your surgeon will put the graft into place using specially designed surgical instruments that will be passed through the other cuts. However, keyhole surgery isn’t suitable for everybody.
Endovascular stent graft replacement
Sometimes aneurysms can be treated using a new procedure called endovascular stent graft replacement (or endovascular aneurysm repair, EVAR). A stent – a tube that is covered with synthetic graft material – is fed through the femoral arteries in your groin up though the aorta to the area of the aneurysm. Your surgeon uses X-ray images to guide the placement of the stent. The graft material bonds with the arterial wall and the blood flows through the stent instead of the weakened aneurysm. However, stents aren’t suitable for everyone – it depends on the location of the aneurysm and other factors. For more information, see endovascular aneurysm repair.
Prevention of thoracic aortic aneurysm
There are several things you can do to reduce your chance of developing atherosclerosis and therefore an aneurysm, such as:
not smoking having your blood pressure and cholesterol checked regularly exercising regularly maintaining a healthy weight eating a healthy diet.
You should also have regular medical check ups if you have a family history of arterial disease so that any problems can be detected early.
This procedure is undertaken with general anaesthesia and will be discussed with your anaesthetist before surgery is carried out- a stay in HDU (high dependency unit) or ITU (intensive therapy unit) is dependant on your medical needs and your recovery from the procedure which will be based on your progress throughout the operation.