In knee replacement surgery (arthroplasty), a damaged, worn or diseased knee is replaced with an artificial joint.
Knee replacement is a routine operation for knee pain when the knee joint has been severely damaged, most commonly by arthritis.
Knee replacement VIDEO
You may consider knee replacement surgery if:
your knee pain is so severe that it interferes with your quality of life and sleep medication and other treatment have not worked or cause severe side effects everyday tasks, such as shopping or getting out of the bath, are difficult or impossible you are feeling depressed because of the pain and lack of mobility you cannot work or have a normal social life
There are two main types of surgery, depending on the condition of the knee: total knee replacement and partial (half) knee replacement.
More than 70,000 knee replacements are carried out in England and Wales each year, and the number is rising. Most people who have a total knee replacement are over 65, and just over half of all patients are women. The Surgery is carried out either by general anaesthetic or by epidural or spinal block that numbs the patient from the waist down. There is a considerable waiting list in the United Kingdom which can sometimes be 18 weeks or more. If you don’t have a private medical policy enabling surgery to be carried out privately in the UK the procedure can cost in excess of up to £10,000. The Ukraine can offer state of the art facilities and procedures carried out by top class experienced orthopaedic surgeons at a cost as little as £4200 which is a saving of up to 87%.
Candidates for knee replacement surgery need to be well enough for both a major operation and the rehabilitation afterwards.
Outlook
Wear and tear through everyday use means that your replacement knee will not last forever. However, for most people it will last for at least 15-20 years, especially if the new knee is cared for properly and not put under too much strain.
Revision knee replacement surgery (replacing the replacement knee) is usually more complicated and a longer procedure than the original surgery. There is no set limit to the number of times you can have revision surgery, but it is widely accepted that the artificial knee joint becomes less effective each time it is replaced.
Research has also shown that patients become less satisfied with their artificial knee each time it is replaced. This is one reason why knee replacement is less likely to be recommended for younger patients.
When it should be done? You may want to consider surgery if:
your knee pain is so severe that it interferes with your quality of life and sleep medication and other treatment have not worked or cause severe side effects everyday tasks, such as shopping or getting out of the bath, are difficult or impossible you are feeling depressed because of the pain and lack of mobility
you cannot work or have a normal social life
You will normally need a knee replacement if you have severe pain, swelling and stiffness in your knee joint and your ability to move the joint is significantly reduced.
A knee replacement is major surgery, so is normally only recommended if non-surgical options have not helped reduce pain or improve mobility.
Knee replacement may be considered for adults of all ages, although young, physically active people are more likely to wear out their replacement joint. As a result, knee replacement is typically recommended for older, less active people as the replacement joint is less likely to wear out and need to be replaced.
Most people who have a total knee replacement are between the ages of 60 and 80. They need to be well enough to cope with both a major operation and the rehabilitation afterwards.The earlier you have a knee replacement, the greater the chance you will eventually need further surgery. However, there is some evidence that having treatment before the knee becomes very stiff leads to a better surgical outcome.
If you are having a knee replacement because of arthritis and also need a hip replacement, the hip should be replaced first as you will need a flexible hip to do the exercises that are necessary after a knee replacement operation.
What should I look for in a specialist?
Choose a specialist who performs knee replacement regularly and can discuss their results with you.
This is even more important if you are having a second or subsequent knee replacement, known as revision knee replacement, which is more difficult to perform. Look for a specialist who will work with you to find the best treatment.
How can I prepare for going into hospital?
Get informed. Find out as much as you can about what is involved in your operation. Your hospital may provide written information or videos.
Arrange help. Arrange for a friend or relative to accompany you on your planned trip and to help you for a week or two after you come out of hospital.
How can I prepare for the operation?
Stay as active as you can. Strengthening the muscles around your knee will aid your recovery. You can be referred to a physiotherapist, who will give you helpful exercises. If you can, continue to gently exercise, such as walking and swimming, in the weeks and months before your operation.
What will happen before the operation?
A couple of weeks before the operation, you will usually be asked to attend a preoperative assessment clinic to meet your surgeon and other members of the surgical team.
They will take a medical history, examine you and organise any tests (such as blood and urine tests), ECG and X-rays needed to make sure you are healthy enough for an anaesthetic and surgery. They will also give you advice on how to prepare for surgery and will ask you about your home circumstances so your discharge from hospital can be planned. If you live alone, have a carer or feel you need extra support, tell the surgical team so that any help or support can be arranged before you go into hospital.
Take a list or packets of any medication you are taking. Some rheumatoid arthritis medications suppress the immune system, which can affect healing. For this reason, you may be asked to stop taking your medication before surgery. Your surgeon can advise you on alternative medications. There may be leaflets, booklets and videos to look at or take away that can give you more information about the operation.
Why knee replacement is necessary
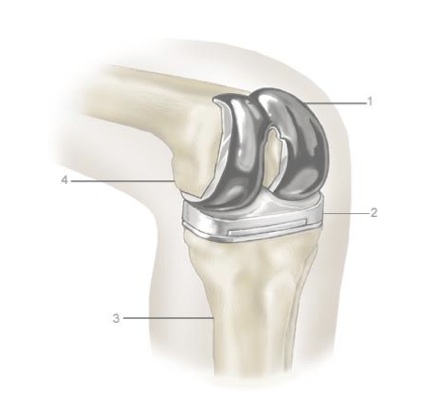
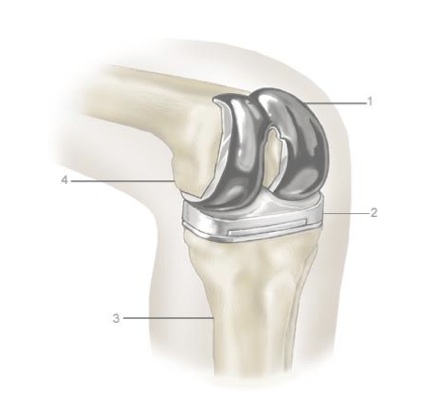
1. Upper prosthesis 2. Lower prosthesis 3. Tibia 4. Femur
Conditions that make knee replacement necessary include:
osteoarthritis rheumatoid arthritis haemophilia gout disorders that cause unusual bone growth (bone dysplasias) death of bone in the knee joint following
Introduction
You are going to have a hip or knee replacement soon. You may have heard that there are several different types of anaesthetic:
a general anaesthetic a spinal anaesthetic an epidural anaesthetic a nerve block (to help with pain afterwards) a combination of anaesthetics.
Your anaesthetist will explain which anaesthetic methods are suitable for you, and help you decide which you would prefer.
A general anaesthetic
A general anaesthetic produces a state of controlled unconsciousness during which you feel nothing. You will receive:
anaesthetic drugs (an injection or a gas to breathe) strong pain relief drugs (morphine or something similar) oxygen to breathe sometimes, a drug to relax your muscles.
You will need a breathing tube in your throat whilst you are anaesthetised to make sure that oxygen and anaesthetic gases can move easily into your lungs. If you have been given drugs that relax your muscles, you will not be able to breathe for yourself and a breathing machine (ventilator) will be used.
When the operation is finished the anaesthetic is stopped and you regain consciousness.
Advantages
You will be unconscious during the operation.
Disadvantages
A general anaesthetic alone does not provide pain relief after the operation. You will need strong pain relieving medicines afterwards which make some people feel quite unwell. Or you may wish to consider a nerve block with a general anaesthetic (see below).
Some of the risks and side effects of general anaesthetics are described later in this booklet. You can get more information about general anaesthetics from the leaflet ‘Anaesthesia explained’ and other leaflets in the series.
A spinal anaesthetic
A measured dose of local anaesthetic is injected near to the nerves in your lower back.
you go numb from the waist downwards you feel no pain, but you remain conscious if you prefer, you can also have drugs which make you feel sleepy and relaxed (sedation).
Advantages – compared to a general anaesthetic
There is some evidence that less bleeding may occur during surgery which would reduce your risk of needing a blood transfusion.
You remain in full control of your breathing. You breathe better in the first few hours after the operation. You do not need so much strong pain relieving medicine in the first few hours after the operation.You should have less sickness and drowsiness after the operation and may be able to eat and drink sooner.
Disadvantages
Some of the risks and side effects of a spinal anaesthetic are described later in this booklet. You can get more information about spinal anaesthetics from the leaflet ‘Your spinal anaesthetic’ (see inside front cover of this leaflet).
An epidural anaesthetic
A small plastic tube (an epidural catheter) is passed through a needle into a place near to the nerves in your back. Through this tube, you receive a measured dose of local anaesthetic and pain relieving drugs. You will experience a reduction of all feeling in your lower body.
Although operations can be done with an epidural alone, it is more commonly used for:
operations expected to be very long, say more than three hours operations expected to be particularly painful afterwards.
For these operations, it is often combined with a spinal or a general anaesthetic.
Advantages
It can be topped up with more local anaesthetic, and therefore its effects can be made to last longer than a spinal anaesthetic.
It can be used to make you comfortable for several days after the operation.
Disadvantages
Not all epidurals are fully effective in relieving pain after the operation. If this happens you will receive additional pain relief.
Some of the risks and side effects of an epidural anaesthetic are described later in this booklet. You can get more information from the leaflet ‘Epidurals for pain relief after surgery’.
A nerve block
This is an injection of local anaesthetic near to the nerves which go to your leg. Part of your leg should be numb and pain-free for some hours afterwards. You may also not be able to move it properly during this time.
If you are having a general anaesthetic, this injection may be done before the anaesthetic starts, or it may be done when you are unconscious.
Advantages
You usually need a lighter general anaesthetic and you should be less sick and drowsy afterwards. This is because you should need less strong pain relieving medicines during and after the anaesthetic.
You should be more comfortable for several hours after the operation.
A combination of anaesthetics
You can have a spinal or epidural anaesthetic and a general anaesthetic together.
You gain the benefits of a spinal or epidural anaesthetic but you are unconscious during the operation The general anaesthetic will be ‘lighter’. Unpleasant after-effects of the general anaesthetic may be less.
You can have a nerve block with a general anaesthetic, or after a spinal anaesthetic.
You should be more comfortable for some hours after the operation than with a general anaesthetic or spinal anaesthetic alone.
Before your operation
You will be asked some questions to check your health before your operation. This may be at a pre-assessment clinic, or it may be by filling in a questionnaire, by talking to the doctors on the ward or by talking to your anaesthetist.
You will be asked about:
your general health and fitness any serious illnesses you have had previous anaesthetics and if there were any problems known to you whether you know of any family members who have had problems with anaesthetics medicines, pills, inhalers or homeopathic remedies that you use any allergies that you have whether you smoke whether you drink alcohol whether you have any loose, capped or crowned teeth.
The anaesthetist’s visit
Your anaesthetist will meet you before your operation and he/she will talk to you about which kind of anaesthetic is suitable for you. This is a good time to ask questions and tell the anaesthetist about any worries that you have. You may find it useful to write down any particular concerns before meeting your anaesthetist so that you don’t forget anything.
You may find that your anaesthetist and the team of staff looking after you have very regular experience of a certain type of anaesthetic and less experience of others. This would add to the advantages of that technique over others.
Your preferences are important. Nothing will happen to you until you understand and agree with what is planned for you. You have the right to refuse if you do not want the treatment suggested.
On the day of your operation
Nothing to eat or drink – fasting (‘nil by mouth’)
The nurses looking after you should give you clear instructions about fasting. It is important to follow these. If there is food or liquid in your stomach during your anaesthetic, it could come up into the back of your throat and damage your lungs.
If you are not having a general anaesthetic, you will still be asked to follow these instructions. This is because a general anaesthetic may be needed unexpectedly, and you need to be prepared.
Having a ‘premed’ (pre-medication)
This is the name for drugs which are given before some anaesthetics.
Some premeds prepare you for the anaesthetic (for example a drug to prevent sickness), others help you to relax. They may also make you more drowsy after the operation. If you want to go home on the same day, this may be delayed. If you think a premed would help you, please ask your anaesthetist.
Your usual medicines
It is important that you continue to take your usual medicines, including inhalers, unless your surgeon or anaesthetist has advised you not to.
Getting ready for theatre
You will be given a hospital gown to put on. Jewellery should be removed or covered with tape to prevent damage to it or to your skin.
You can wear your hearing aid, glasses and dentures until you are in the anaesthetic room. If you are not having a general anaesthetic, you can usually keep them on during the operation.
If you are having a hip replacement you will need to take off your pants. If you are having a knee replacement you may be able to keep them on, or you may be given paper pants to wear.
In the anaesthetic room
This is the room next to the operating theatre. Several people will be there, including your anaesthetist and an anaesthetic assistant.
The anaesthetist will use equipment to measure:
your heart rate – three sticky patches on your chest (electrocardiogram or ECG) your blood pressure – a cuff on your arm the oxygen level in your blood – a clip on your finger (pulse oximeter).
A needle is used to put a thin soft plastic tube (a cannula) into a vein in the back of your hand or arm. Drugs and fluids can be given through this cannula.
If needles worry you, please tell your anaesthetist. A needle cannot usually be avoided, but there are things he or she can do to help.
During the operation
All anaesthetics may cause changes in:
your heart rate your blood pressure your breathing.
Changes may also occur due to loss of blood, the use of surgical cement and the use of a tourniquet on your leg (knee replacements only).
Your anaesthetist may intentionally adjust your blood pressure and breathing to control your response to surgery. General anaesthetic drugs are given continuously throughout surgery and are stopped when the operation ends. A spinal, epidural or nerve block injection will wear off some hours after the operation is finished.
An anaesthetist will stay with you for the whole operation and watch your condition very closely, adjusting the anaesthetic as required.
After the operation
You will be taken to the recovery room, which is near to the operating theatre.
You will have your own nurse in the recovery room. You will not be left alone.
There will be other patients in the same room.
You may need to breathe oxygen through a light plastic mask.
You will have a drip (a bag of sterile water with added salt or sugar which is attached to your cannula and drips slowly into a vein).
Your blood pressure, heart rate and oxygen level will be measured. If you have pain or sickness, the nurse will treat it promptly.
When the recovery room staff are satisfied that you have recovered safely from your anaesthetic you will be taken back to the ward.
Pain relief
Good pain relief is important and some people need more pain relief medicines than others. Here are some ways of giving pain relief:
Patient controlled analgesia (PCA)
This is a method using a machine that allows you to control your pain relief yourself. Small doses are given into a vein for immediate effect.
Injections
These are given into a vein for immediate effect, or into your leg or buttock muscle. Strong pain relieving drugs such as morphine, pethidine and codeine may be given by injection.
Pills, tablets or liquids to swallow
These take at least half an hour to work and you need to be able to eat and drink and not feel sick for these drugs to work.
Suppositories
These waxy pellets are placed in your back passage (rectum). They are useful if you cannot swallow or might vomit.
Nerve blocks and epidurals
As already described, these can give effective pain relief for hours or days after the operation.
You can get more information about pain relief from:
The nurses on the ward
Your anaesthetist
The pain-relief team – some hospitals have a team of nurses and doctors who specialise in the relief of pain after surgery. You may be able to contact this team for advice before you come into hospital. Leaflets may be available about pain relief methods.
Manufacturers’ information leaflets for patients about any drug you are offered (your nurses should be able to give you these leaflets).
Side-effects, complications and risks
In modern anaesthesia serious problems are uncommon. Risk cannot be removed completely, but modern equipment, training and drugs have made anaesthesia a much safer procedure in recent years.
Common and very common side effects
All anaesthetics
Pain around injection sites and general aches and pains
You may not be able to pass water (urine) or you may wet the bed. This is because you are lying down, you may have pain and you may have received strong pain relieving drugs. A soft plastic tube may be put in your bladder (a catheter) to drain away the urine for a day or two. This is more common after spinal or epidural anaesthetics.
Spinal or epidural anaesthetics
You will not be able to move your legs properly for a while. If pain-relieving drugs are given in your spinal or epidural as well as local anaesthetic, you may feel itchy and/or sick.
General anaesthetics
Sickness – treated with anti sickness drugs Sore throat or damage to lips or tongue – treated with pain relief drugs Drowsiness, headache, shivering, blurred vision – may be treated with fluids or drugs Difficult breathing at first – this usually improves rapidly Confusion and memory loss are common in older people, but are usually temporary.
Uncommon side effects and complications General anaesthetics
Damage to teeth Chest infection
Awareness (becoming conscious during a general anaesthetic)
Rare or very rare complications All anaesthetics
Serious allergic reactions to drugs Damage to nerves
General anaesthetics
Damage to eyes Vomit getting into your lungs
Frequently asked questions
Q Should I take all my usual medicines or tablets right up to my operation?
Your surgeon and anaesthetist will tell you which drugs they would like you to take and which ones to stop. It helps if you bring all your medication with you so they know what you usually take.
Q Do other drugs affect the anaesthetic?
Most drugs that treat heart, circulation or breathing problems have some effect on the anaesthetic. Your anaesthetist will be familiar with all the drugs that you take and will adjust the anaesthetic accordingly.
Q How do you know how much anaesthetic each person needs?
The amount of anaesthetic needed for a spinal or general anaesthetic varies with your age, your weight and build and your general health. There is no easy formula! Anaesthetists use their judgment and experience. They stay with you all the time and they adjust the anaesthetic as needed.
Q Can I bring a relative or friend with me?
It may be possible to arrange this. If this would help you, please ask the nurses on the ward or your anaesthetist if a relative or friend could come into the anaesthetic room.
Q How long does it take to regain consciousness after a general anaesthetic?
You regain consciousness in 5 – 20 minutes. It may be longer before your memory fully returns.
Q Am I likely to get long-term backache if I have a spinal injection?
You may have a bruise at the site of the injection, but this soon passes. Backache due to arthritis is common in people having a hip or knee replacement. It is not made worse by having a spinal or epidural injection.
Questions you may like to ask your anaesthetist
Who will give my anaesthetic? What type of anaesthetic do you recommend? Have you often used this type of anaesthetic? What are the risks of this type of anaesthetic? How will I feel afterwards?

